Can Outdoor Access Reduce the Risk of Dementia?
A new study links nearby green spaces to lower hospitalizations

Photo by Zinkevych/iStock
For years we’ve been taught that “brain workouts”—daily crossword puzzles, learning a foreign language, playing a musical instrument—can strengthen our minds, improve our memory, and stave off dementia. But what about taking a walk? Simply stepping out for some fresh air? A recent study suggests that spending more time in nature may also help older people delay serious neurodegenerative diseases.
The study found that living near green space—parks, forests, grasslands, fields, street trees, and even desert—can help protect against some risks associated with dementia. The study of nearly 62 million Medicare beneficiaries discovered that older adults who lived in areas with more green space had a lower rate of hospitalization related to Alzheimer’s disease, Parkinson’s, and related dementias (such as Lewy body dementia and vascular dementia).
The reasons for this remain unclear, but Jochem Klompmaker, author of the study and a postdoctoral research fellow at the Harvard T.H. Chan School of Public Health, said the boost might be linked to healthier lifestyle choices encouraged by easier access to the outdoors. “Dementia is affected by age and genetics,” Klompmaker said. “You can’t modify those factors, unfortunately. . . . [But] there’s increasing evidence that a healthy lifestyle can slow your risk—and living near green space can encourage a healthier lifestyle.”
Don Elbert, an associate professor of neurology at the University of Washington, who was not involved in the research, said living near green spaces might lead to higher levels of physical activity and also be correlated with fewer pollutants. “The combination of those two things is definitely helpful,” Elbert said, but noted that such lifestyle changes could only slow, not stop, disease progressions.
“My favorite study on physical activity and Alzheimer’s looks at a group of people with genetic mutations that lead to Alzheimer’s disease at a fairly well-defined age,” he said. “In this group, two and a half hours of exercise a week delayed their onset of symptoms. So yes, I think exercise is a key component, but it’s important to keep in mind that physical activity delayed the onset; it didn’t prevent it.”
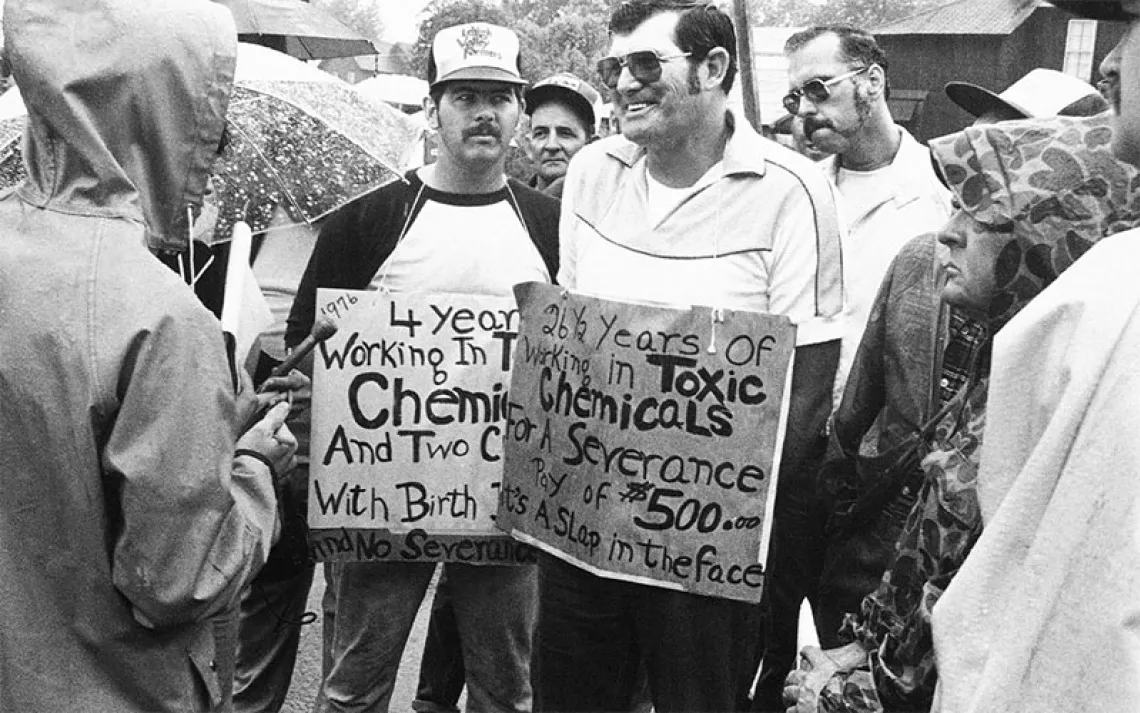
Still, links between access to healthy environments, green spaces, and dementia risk go beyond exercise; fine particulate matter (PM2.5), essentially soot, has long been associated with increased rates of Alzheimer’s and Parkinson’s. Exposure to pesticides and heavy metals has also been implicated. One study in Scotland found that spending time in woodlands led to increased feelings of well-being for people with dementia.
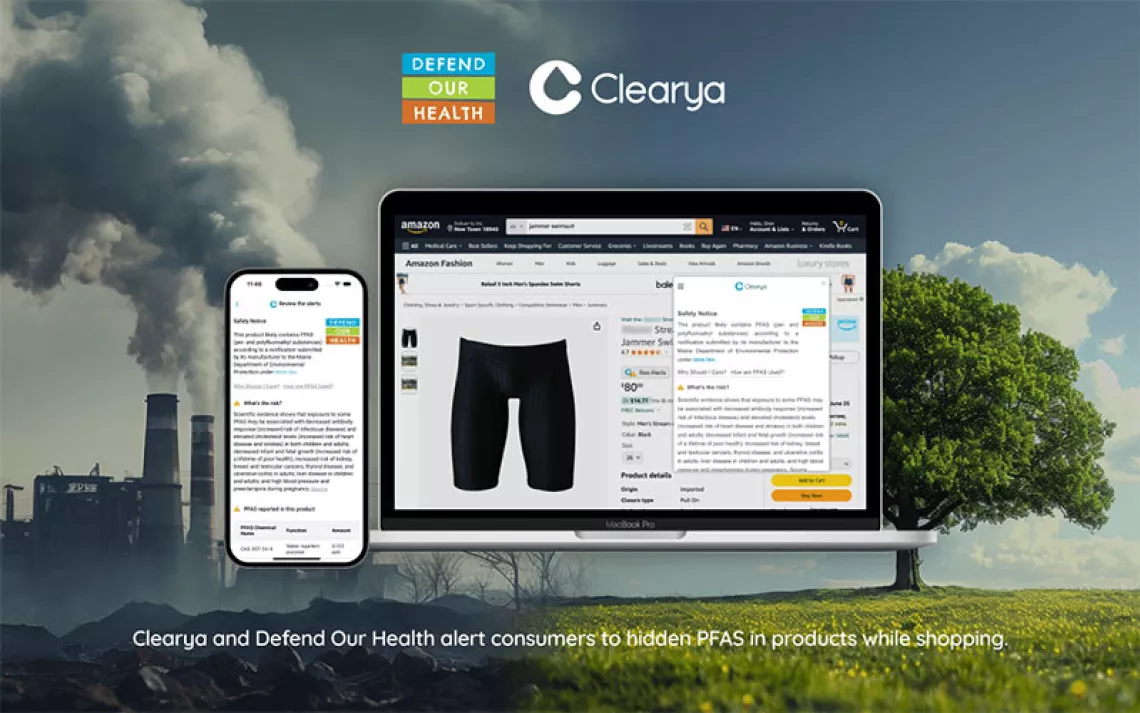
And by analyzing green space and park cover—and then comparing them with dementia-related hospital admissions—Klompmaker and his colleagues captured a bigger picture, one that carries implications for social justice. There is a “nature equity gap” in the United States, where people of color and low-income communities are less likely to have safe and accessible ways to get outside.
A second study, published in January, looked at racial, ethnic, and socioeconomic disparities and natural environments combining US Census tracts (2015–2019) with the same satellite data. Tracts with higher socioeconomic status had higher greenness and park cover. “We know there are health disparities between these groups; they might be partially explained by lower natural environment exposures,” Klompmaker said.
In the US, some 6.5 million people over 65, of whom a disproportionate number are women and people of color, already have Alzheimer’s. Due to a shortage of elder-care infrastructure and workers, many will endure the disease with far too little support.
In spite of the obvious benefits of spending time outdoors, in practice, access to nature is often denied people with dementia, who either have limited means of leaving their own homes, or if they live in a care facility, find that the doors are locked. In a world with a rapidly aging population where dementia has been identified as a global health priority, rights to fresh air and access to dementia-friendly open spaces are increasingly seen not only as good practice in elder care but also a matter of rights and social justice.
At the same time, a 2020 National Institutes of Health study found that while engagement in green spaces has a positive impact on well-being and quality of life, little is known about the impacts of green space access specifically for people with dementia, who have an urgent and heightened need to maintain a quality of life.
Findings did show, however, that gardens and horticultural programs, urban woodlands, parks, and neighborhood outdoor environments can impact dementia patients in several ways, from reinforcing identity and healthy risk-taking to empowerment and meaningful activities—and that these factors are all worthy of consideration by policy makers and caregivers.
In southwestern France, the Village Landais is part of a growing trend to make memory-care facilities less like hospitals and more like small neighborhoods. Just 120 residents live full-time on 17 acres in group homes where they can walk freely on loops through the lush green property, tend to a large garden each morning, and feed two pet donkeys. Although every resident of the village has dementia, they have the autonomy to spend each day however they choose—and many choose to be outdoors.
Every first Friday in Seattle, a different public garden hosts a Garden Discovery Walk in partnership with the University of Washington Memory and Brain Wellness Center. The group explores a garden or community P-Patch and engages in a nature-inspired activity. The walks are free for people with memory loss and their partners, and a chance for people living with dementia to “get their hands dirty” in a gardening project and explore green spaces in a supportive environment.
At the Portland Memory Garden, one of eight memory gardens in the US, paths take visitors by fragrant plants that are interesting to smell and touch, and the staff intentionally grows red geraniums, daisies, and marigolds because those are the flowers they’ve found that trigger memories for people who were children 70 years ago and now live with dementia.
These dementia-friendly nature programs are all part of a growing grassroots movement in horticultural memory-loss therapy: the bold idea that rich sensory outdoor experiences can be a specific treatment for dementia, allowing those with memory loss to live more in the present, where tree canopy, bright flowers, and leafy green plants help them flourish on their own terms.
 The Magazine of The Sierra Club
The Magazine of The Sierra Club